Wound
A wound is a type of injury in which skin is torn, cut, or punctured (an open wound), or where blunt force trauma causes a contusion (a closed wound). In pathology, it specifically refers to a sharp injury that damages the dermis of the skin.
Classification
Open
Open wounds can be classified according to the object that caused the wound. The types of open wound are:
- Incisions or incised wounds, caused by a clean, sharp-edged object such as a knife, razor, or glass splinter.
- Lacerations, irregular tear-like wounds caused by some blunt trauma. Lacerations and incisions may appear linear (regular) or stellate (irregular). The term laceration is commonly misused in reference to incisions.
- Abrasions (grazes), superficial wounds in which the topmost layer of the skin (the epidermis) is scraped off. Abrasions are often caused by a sliding fall onto a rough surface.
- Avulsions, injuries in which a body structure is forcibly detached from its normal point of insertion. A type of amputation where the extremity is pulled off rather than cut off.
- Puncture wounds, caused by an object puncturing the skin, such as a nail or needle.
- Penetration wounds, caused by an object such as a knife entering and coming out from the skin.
- Gunshot wounds, caused by a bullet or similar projectile driving into or through the body. There may be two wounds, one at the site of entry and one at the site of exit, generally referred to as a “through-and-through.”
Closed
Closed wounds have fewer categories, but are just as dangerous as open wounds. The types of closed wounds are
- Contusions, more commonly known as bruises, caused by a blunt force trauma that damages tissue under the skin.
- Hematomas, also called a blood tumor, caused by damage to a blood vessel that in turn causes blood to collect under the skin.
- Crush injury, caused by a great or extreme amount of force applied over a long period of time.

An open wound

A laceration to the leg

A lacerated knee

An infected puncture wound to the bottom of the forefoot.

A puncture wound from playing darts.
Pathophysiology
To heal a wound, the body undertakes a series of actions collectively known as the wound healing process.
Management

Wound, sewn with four stitches
The overall wound treatment in Delhi depends on the type, cause, and depth of the wound as well as whether or not other structures beyond the skin (dermis) are involved. Treatment of recent lacerations involves examining, cleaning, and closing the wound. Minor wounds, like bruises, will heal on their own, with skin discoloration usually disappearing in 1–2 weeks. Abrasions, which are wounds with intact skin (non-penetration through dermis to subcutaneous fat), usually require no active treatment except keeping the area clean, initially with soap and water. Puncture wounds may be prone to infection depending on the depth of penetration. The entry of puncture wound is left open to allow for bacteria or debris to be removed from inside.
Cleaning
Evidence to support the cleaning of wounds before closure is poor. For simple lacerations, cleaning can be accomplished using a number of different solutions, including tap water and sterile saline solution. Infection rates may be lower with the use of tap water in regions where water quality is high. Cleaning of a wound is also known as wound toilet.
Closure
If a person presents to a healthcare center within 6 hours of a laceration they are typically closed immediately after evaluating and cleaning the wound. After this point in time, however, there is a theoretical concern of increased risks of infection if closed immediately. Thus some healthcare providers may delay closure while others may be willing to immediately close up to 24 hours after the injury. A single study has found that using clean non sterile gloves is equivalent to using sterile gloves during wound closure.
If closure of a wound is decided upon a number of techniques can be used. These include bandages, a cyanoacrylate glue, staples, and sutures. Absorbable sutures have the benefit over non absorbable sutures of not requiring removal. They are often preferred in children. Buffering the pH of lidocaine makes the freezing less painful.
Adhesive glue and sutures have comparable cosmetic outcomes for minor lacerations 5 cm in adults and children. The use of adhesive glue involves considerably less time for the doctor and less pain for the person with the cut. The wound opens at a slightly higher rate but there is less redness. The risk for infections (1.1%) is the same for both. Adhesive glue should not be used in areas of high tension or repetitive movements, such as joints or the posterior trunk.
Dressings
The effectiveness of dressings and creams containing silver to prevent infection or improve healing is not currently supported by evidence.
Imaging
A wound may be recorded for follow-up and observing progress of healing with different techniques which consist of, but not limited to:
- Photographs, with subsequent area quantification using computer processing
- Wound tracings on acetate sheets
- Kundin wound gauge
Complications

The patient has a deep wound at the knee, and radiography is used to ensure there is no hidden bone fractures.
Bacterial infection of wound can impede the healing process and lead to life threatening complications. Scientists at Sheffield University have identified a way of using light to rapidly detect the presence of bacteria. They are developing a portable kit in which specially designed molecules emit a light signal when bound to bacteria. Current laboratory-based detection of bacteria can take hours or even days.
Workup
Individuals who have wounds that are not healing should be investigated to find the causes. Many microbiological agents can be responsible for this. The basic workup includes evaluating the wound, its extent and severity. Cultures are usually obtained both from the wound site and blood. X rays are obtained and a tetanus shot may be administered if there is any doubt about prior vaccination.
Chronic
Non-healing wounds of the diabetic foot are considered one of the most significant complications of diabetes, representing a major worldwide medical, social, and economic burden that greatly affects patient quality of life. Almost 30 million Indians-one in every 10-are diabetic and the disease is causing widespread disability and death at an epidemic pace. Of those with diabetes, 6.5 million are estimated to suffer with chronic or non-healing wounds. Associated with inadequate circulation, poorly functioning veins, and immobility, non-healing wounds occur most frequently in the elderly and in people with diabetes-populations that are sharply rising as the nation ages and chronic diseases increase and thus it requires proper diabetic foot treatment in Delhi.
Although diabetes can ravage the body in many ways, non-healing ulcers on the feet and lower legs are common outward manifestations of the disease. Also, diabetics often suffer from nerve damage in their feet and legs, allowing small wounds or irritations to develop without awareness. Given the abnormalities of the microvasculature and other side effects of diabetes, these wounds take a long time to heal and require a specialized treatment approach for proper healing.
As many as 25% of diabetic patients will eventually develop foot ulcers, and recurrence within five years is 70%. If not aggressively treated, these wounds can lead to amputations. It is estimated that every 30 seconds a lower limb is amputated somewhere in the world because of a diabetic wound. Amputation often triggers a downward spiral of declining quality of life, frequently leading to disability and death. In fact, only about one third of diabetic amputees will live more than five years, a survival rate equivalent to that of many cancers.
Many of these lower extremity amputations can be prevented through an interdisciplinary approach to treatment involving a variety of advanced therapies and techniques, such as debridement, hyperbaric oxygen treatment therapy, dressing selection, special shoes, and patient education. When wounds persist, a specialized approach is required for healing.





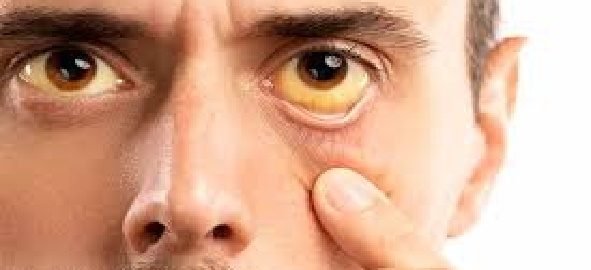
 Accumulation of bile pigments in the tissues, which in the examination can be seen by the yellow tone of the skin and the conjunctiva, which occurs when there is an obstacle, to the evacuation of the bile, in the bile canaliculus under the microscope (for example, due to primary biliary cirrhosis), in the intrahepatic bile ducts (for example, by sclerosing cholangitis) or in the main bile ducts (for example, choledocholithiasis, tumors, etc.).
Accumulation of bile pigments in the tissues, which in the examination can be seen by the yellow tone of the skin and the conjunctiva, which occurs when there is an obstacle, to the evacuation of the bile, in the bile canaliculus under the microscope (for example, due to primary biliary cirrhosis), in the intrahepatic bile ducts (for example, by sclerosing cholangitis) or in the main bile ducts (for example, choledocholithiasis, tumors, etc.).
















