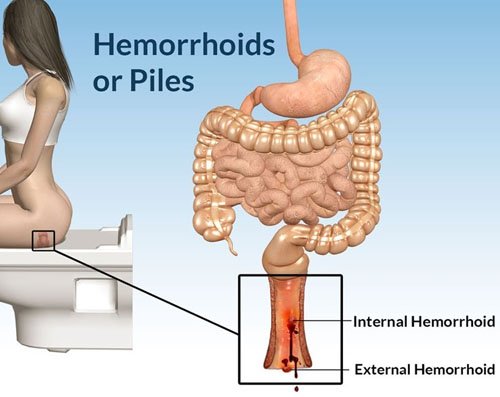
Anal fistula treatment in Delhi is done for a very painful fistula appeared near the anus. A fistula is an abnormal connection (formation of a channel) between two parts, which occurs inside the body. It can be formed between two organs, between the intestine and another structure, between two blood vessels, between an artery and a vein, and so on. In the specific case of an anal fistula, a tube-shaped duct forms under the skin surrounding the anus. It consists, therefore, of an external orifice (in the skin of the anus) and an internal one (inside the anus or rectum) existing communication between both, although there are complex fistulous trajectories that do not communicate these orifices. They are usually the consequence of an anal abscess that has evolved in most cases.
An anal fistula is a relatively common disease, especially in adults, although it can occur in children if it is associated with intestinal inflammatory diseases such as Crohn’s disease. It appears more frequently in males than in females. Its prevalence is estimated at around 30%, with a peak of age around 40 years.
The clinical picture of this disorder can be practically asymptomatic if it is in a zone somewhat distant from the anus, with mild discomfort of itching or stinging, or manifest as a sharp pain, very intense and cutting nature that occurs at the time of passage of the stool in the area during the deposition, and that may remain for several hours after the same. Occasionally there may be slight bleeding and small amounts of pus.
Causes
In general, an anal fistula can be caused by the presence of some type of wound, an injury produced during surgery, infection or inflammation. The obstruction of a gland is the situation that is most commonly associated with the formation of fistulas.
The accumulation of any liquid in a body cavity favors the appearance of infections so that if the secretion product of the anal glands does not find an exit route it is very likely that the enteric bacteria (bacterial flora found in the intestine of healthy individuals) provoke an infection in a short time. Immediately, pus begins to form and accumulate, forming an abscess (very localized lesion, characterized by the accumulation of pus inside it) that usually ends up draining at some point in the anus. This is the cause of approximately 80-90% of cases.
The abscesses in this area may also be formed by the infection of an anal fissure (small break in the mucus covering the anus) or a sexually transmitted infection contact.
Symptoms
The most frequent symptoms for which a person with anal fistula consults the laparoscopic surgeon in Delhi are a pain in the area of the anus and the presence of pus or drainage of some malodorous secretion.
On many occasions, these individuals have previously consulted for infections of the area or true abscesses. Or have presented pain and pus secretion for a long time, but have not consulted because the symptoms were intermittent or modesty.
The pain is variable in intensity, being able to accentuate when defecating when sitting down, or on other occasions when coughing or sneezing due to the increase of pressure generated by these situations. As a difference from other pathologies in this region, the pain generated by abscesses or fissures is usually more intense, besides having a red and hard lump in the case of abscesses.
You can see the external orifices of the fistula, sometimes several, through which it expels purulent, malodorous, sometimes even fecaloid (vomit of fecal material) content. This secretion usually causes irritation of the perianal skin, presenting itching, stinging and redness of the area.
When the laparoscopic surgeon in Delhi digitally explores the anal and rectal area, it can identify which type of fistula is attending the classification described at the beginning, depending on the relationship with the external and internal sphincter, as well as estimate the length and complexity of the fistulous tract.
Diagnose
A physical examination will be carried out in the first instance to the patient who comes to consult with discomforts that may make us suspect the presence of an anal fistula. The doctor will look for the presence of abscesses and openings in the skin that shows the existence of an anal fistula. Normally a zone of reddened skin will be observed and painful to the touch. If it is found, it will try to define its route and depth with the help of a probe.
The presence of fistulas is not always evident since the lesion does not have to be on the surface of the skin. For this reason, it is sometimes necessary to perform a digital rectal examination and observe the anal canal and rectum with the help of an anoscope; This instrument is a short and rigid tube with a light at the end, which allows to observe the inside of the cavity and take samples.
An important point in the diagnosis of an anal fistula is to find its origin. Since there are other pathologies that can lead to the appearance of abscesses and fistulas, to determine if the underlying cause is, for example, some type of cancer, Crohn’s disease or other pathology, a sigmoidoscope examination will be performed (sigmoidoscopy). This instrument is a long and flexible tube that allows you to see the large intestine up to 60 cm inward from the anus.
On other occasions anal or endoanal ultrasound is useful by means of a rotating probe to determine the path, route, presence of other secondary paths and collections of pus.
At present, magnetic resonance imaging is also available to obtain information on the characteristics of the fistula or fistulas and their complexity, as well as the presence of adjacent complications. TAC can also be used if contrast is added to supplement the study.
Anal Fistula Treatment in Delhi
The only effective anal fistula treatment in Delhi for those patients who suffer it is surgical intervention. By means of this procedure, it is intended to definitively eliminate the fistula and correct the alterations that may have appeared as a result of it, without compromising the anal continence. The disappearance of the fistula implies the disappearance of the associated painful discomfort, inflammation, suppuration …
Depending on the type of fistula, its path, depth, etc., different types of intervention may be performed.
- Fistulotomy: it consists of the opening and emptying of the fistulous tract, trying to ensure healing as efficiently and quickly as possible.
- Fistulectomy: this anal fistula treatment in Delhi involves the complete removal of the fistulous tract. The drawback with respect to the prior art is that it gives rise to larger wounds and, therefore, the healing is slower and more expensive.
- Sedal or seton: there are three variants of this technique depending on the objective of the intervention.
- Cutting seton: the objective of this modality is the elimination of the fistula. It is done by passing through its surgical silk that is tightened gradually so that the silk section the sphincter but at the same time this has enough time to go scarring.
- Drainage seton: performed to drain pus or debris from the fistula; in this way, the formation of a new abscess will be avoided. This silk will be placed through the fistula, and once the drainage process is complete it allows surgical repair even in the absence of infection.
- Seton guide: it is placed in the same way as the previous one. Its function is to keep the fistulous tract patent until the patient can be definitively operated on. This method is usually used in patients with recurrent perianal abscesses, in which the point where the abscess was found cannot be identified since there is no sequela of the fistulous tract.
In the case of anal fistulas related to Crohn’s disease, the initial anal fistula treatment in Delhi is not surgery, but the management with metronidazole antibiotics, to avoid the operating theater, as well as to reinforce the systemic treatment of the disease with azathioprine-type immunosuppressants or agents. biological agents such as adalimumab or infliximab. The techniques described above are resorted to if they fail.
For pain relief prior to and after the intervention, analgesics and common anti-inflammatories will be useful, and it is important to achieve non-painful defecation through proper hydration and an adequate supply of fiber to the diet.
Prevention
The prevention of anal fistulas implies the prevention of all those factors that can trigger them:
- Fissures. In adults, it is common to have fissures due to constipation or prolonged diarrhea. It is important to have a balanced diet, rich in fiber, to ensure proper intestinal transit, and avoid foods that may cause irritation.
- The appearance of fissures and perianal abscesses is also common in babies. To prevent them it is advisable to change diapers often and clean it properly.
In addition, usual measures should be taken into account such as:
- Clean after defecation with soft materials or water.
- Avoid a sedentary lifestyle; the physical activity strengthens the immune system.
- Use prophylactic measures when having sex.
It is important to consult a laparoscopic surgeon in Delhi when you perceive anal pain and spotting of underwear or non-fecal material with a bad smell, to avoid that in the case of abscesses, these evolve to the formation of the fistula.
In addition to these basic measures, you can try some homeopathic practices, not as a treatment, but as a prevention or as a way to acquire healthier habits, in order to avoid the reappearance of injuries already treated. With regard to food, there are for example certain foods that are attributed anti-inflammatory properties (ginger, turmeric, vegetables, and fruits), refined products such as sugar, fried foods, and other processed foods have the opposite effect, therefore, It may be beneficial to reduce your consumption.







 Obesity is today one of the main concerns of the World Health Organization (WHO). Already considered as a pandemic, overweight and obesity in India have alarming rates, leading the rankings internationally. Every year thousands of people opt to go for
Obesity is today one of the main concerns of the World Health Organization (WHO). Already considered as a pandemic, overweight and obesity in India have alarming rates, leading the rankings internationally. Every year thousands of people opt to go for